“Arthritis” is a term used to describe a wide range of conditions that negatively impact the musculoskeletal system. The word arthritis is Greek for joint inflammation, one of the defining symptoms of the disease.
All patients suffering from arthritis will experience some level of discomfort and pain. Arthritis pain varies in severity and duration depending on the underlying cause, disease progression, and trigger events.
SUMMARY
With more than 100 different variations of the disease, there are slight, but important differences in symptoms. Managing these symptoms takes a multi-disciplinary response. Each patient will need a different approach based on the type of arthritis they have and their individual circumstances.
Overarching arthritis symptoms
Joint stiffness
Stiffness is the feeling that the motion of a joint is limited or difficult. The feeling is not caused by weakness or reluctance to move the joint due to pain.
Joint swelling
The swelling may cause the joint to appear larger or abnormally shaped.
Joint tenderness
Joint pain or tenderness refers to discomfort, aches, and soreness in any of the body’s joints.
Impaired joint function and mobility
Impaired joint mobilityrefers to a weakened or inability to move the joints through a full range of motion.
Fatigue and malaise
Malaise is a feeling of weakness, overall discomfort, illness, or simply not feeling well.
Difficulty sleeping
Arthritis symptoms can affect your ability to fall asleep, stay asleep, and get enough sleep. It can also impact your bed partner’s sleep.
These arthritis symptoms may then give way to secondary symptoms such as reduced flexibly, poor aerobic fitness, and muscle weakness. The symptoms of arthritis can have a significant impact on quality of life, making normally easy daily activities challenging.
Arthritis types and their associated symptoms
While there are many different arthritis classifications, some are more prevalent than others.
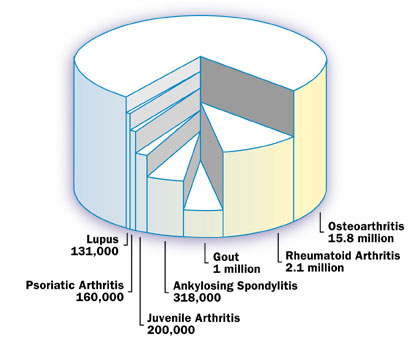
Osteoarthritis and rheumatoid arthritis are by far the most common forms of arthritis affecting 80% and 10% of all patients respectively.
Gout (5%), ankylosing spondylitis (1.6%), juvenile arthritis (1%), fibromyalgia, psoriatic arthritis (0.8%) and systemic lupus erythematosus (SLE, 0.7%) are also among the most diagnosed types forms of the disease after osteoarthritis and rheumatoid arthritis.
Arthritis distribution by type
In the United Kingdom almost 9 million people have sought treatment for osteoarthritis. It is the most common form to arthritis.
Although osteoarthritis can affect any joint, the major weight-bearing joints tend to be the most affected. The knee is most prevalent site, followed by the hip.
In the United States, research suggests that almost half the adult population will have symptomatic knee arthritis by the time they reach 85 years of age1. The same study has also suggested that two in every three obese people are likely to develop knee osteoarthritis at some stage throughout their life.
Debilitating hip osteoarthritis is estimated to affect 25% of adults at some stage of their life2. These are all direct effects of widespread obesity in modern society.
According to statistics from Arthritis Research UK, in England, osteoarthritis of the knee affects approximately 18% of the population. Osteoarthritis of the hip affects 11% of the population aged 45 and older.
Osteoarthritis Symptoms
Osteoarthritis is a degenerative joint disease. In addition to the knee and hips, other joints typically affected include the lower back, ankles, neck, and the small joints with the hands. This disease usually occurs in joints that have been injured. This could be from an accident, repeated overuse, or a sporting injury.
The damage gradually wears away the cartilage cushioning the joint, causing the bones to rub together. Although the specific causes of the disease are not fully understood, it’s thought to be the result of both molecular and mechanical actions within the joint.
The onset of the disease is very gradual. Initially patients may notice stiffness of the affected joint, especially in the morning. As the disease progresses, stiffness will become more common, joint swelling and pain will increase, and mobility will be impaired. In addition to the stiffness, swelling and pain symptoms, there will also be radiographic changes, with the narrowing of the joint space, bony sclerosis, and osteophyes.
It can take many years before joints affected by osteoarthritis fail and with the right arthritis treatments it’s possible to slow the disease progression. Current treatments focus on improving joint function and relieving symptoms.
This may include a special arthritis diet, weight control, physical therapy, use of supplements and medications, plus patient education. Eventually a total joint replacement may be required.
Rheumatoid arthritis prevalence and symptoms
Following osteoarthritis, rheumatoid arthritis is the second most common form of arthritis. The most common type of inflammatory arthritis rheumatoid arthritis affects approximately 400,000 people in the UK according to the National Health Service (NHS) and is also the most common type of type of inflammatory joint disorder. Adults of any age can be affected by this condition, although it most commonly develops between the ages of 40 and 50.
The immune system sends antibodies to the joints where they attack the synovial membrane. The resulting inflammation causes the release of enzymes that start to damage the bones, cartilage, tendons, and ligaments. This eventually leads to joint degradation and physical alteration of the shape and alignment of the affected joint.
The onset of the disease usually starts between the ages of 30 and 50; however it can develop at any age. Women are more likely to suffer from rheumatoid arthritis compared with men.
Rheumatoid arthritis symptoms
Symptoms of rheumatoid arthritis tend to develop gradually, marked by swelling and stiffness of the joints and associated pain. Often the feet and hands are affected first, before the arthritis spreads to other joints in the body. Shoulders, elbows, hips, and knees are frequently affected by this inflammatory disease.
People affected by rheumatoid arthritis usually find mornings the worse. This is when the joints are at their stiffest. Usually symptoms reduce as the day progresses and the affected joints loosen up. Other symptoms may include redness and excessive heat around the joint, loss of appetite, fatigue, and rheumatoid nodules.
Approximately 20-35% of people with rheumatoid arthritis develop rheumatoid nodules.
These are firm tissue lumps that can occur close to the affected joint(s).
They are most commonly found on the hands, fingers, knuckles, and elbows. Some people find the nodules painful and they can interfere with daily activities. Other people don’t have any problems with the nodules.
People with rheumatoid arthritis who also smoke have a much higher risk of developing rheumatoid nodules3. There is also an increased risk of nodule development in rheumatoid arthritis patients taking the immune suppressant drug Methotrexate4.
The severity of rheumatoid arthritis symptoms and how fast the disease develops will vary from person to person. Often people find that their symptoms will come and go.
Flare-ups are common and may follow a noticeable pattern. While there isn’t a cure, it’s possible to better manage the symptoms using a combination of supplements, diet, exercise and medications.
Juvenile arthritis prevalence and symptoms
This is a misconception that arthritis is an older person’s disease, because it affects young people as well.
In the United Kingdom approximately 12,000 children under the age of 16, equivalent to 1 in 1,000 children suffer from some type of arthritis. It most commonly occurs in children aged between 7 and 12, although it can also affect infants and older adolescents.
Childhood arthritis is often termed as juvenile idiopathic arthritis.
The disease is further classified into three broad groups oligoarticular, polyarticular, or systemic.
Of these three forms, oligoarticula juvenile idiopathic arthritis is the most common type, accounting for approximately 60% of cases. Girls are more likely to experience juvenile idiopathic arthritis compared with boys. Some forms of this disease can last for months, while others will last indefinitely.
Juvenile arthritis symptoms
Oligoarticular juvenile idiopathic arthritis affects four or less joints. Knees and/or ankles are often affected and subjected to painful swelling.
It can even affect other organs, such as the eyes5. Polyarticular juvenile idiopathic arthritis has similar symptoms, although it affects many more joints in the body. It most commonly develops before the age of seven, although can also occur later in adolescents.
Systemic juvenile idiopathic arthritis initiates with systemic symptoms such as rashes, lethargy, fever, and enlarged glands. Often these early signs are mistakenly diagnosed as an infection.
Joint and muscle pain are also common symptoms. This type of juvenile idiopathic arthritis usually affects children before the age of five.
Diagnosing juvenile arthritis
Diagnosing juvenile idiopathic arthritis can be difficult because many of the symptoms presented also accompany other illnesses. Constant swelling and pain of the joints, accompanied by unexplained fever, skin rashes, and swollen lymph nodes are key signs. To make a diagnosis, doctors will assess symptoms, perform laboratory test, x-rays, physical examinations, and take into account family history.
Like all other forms of arthritis there is no cure. Treatment options are similar to those which are offered to adults. Exercise is especially helpful. Making dietary changes may also assist in reducing inflammation and stress on the joints. How juvenile arthritis is treated will depend on individual circumstance and symptoms.
Fibromyalgia prevalence and symptoms
Fibromyalgia is poorly understood. It has no known aetiology (causes), prognosis, cure, or clear diagnostic criteria. An overarching term, fibromyalgia is used to describe a group of symptoms which include muscle stiffness and generalised pain. It is a long-term condition that affects approximately 1 in every 25 people.
Women are more susceptible to fibromyalgia than men. The condition can vary considerably between person to person and from day to day. Many people experience flare-ups, with symptoms becoming much worse during these times.
Unlike osteoarthritis or rheumatoid arthritis, fibromyalgia isn’t degenerative of inflammatory. Although it can cause severe pain and disrupt daily life, studies suggest that it isn’t a progressive disease, and doesn’t cause long-term damage to the joints of muscles.
Fibromyalgia symptoms
Fibromyalgia can affect many different areas of the body.
Common symptoms include aching and stiffness in muscles, extreme fatigue, cognitive dysfunction, and sleep disturbances.
Other less frequent symptoms may include autonomic dysfunction, mood swings, headaches and/or migraines, and an irritable bowel. In many cases, people with this condition find that their body aches all-over.
Unfortunately there are no definitive tests to confirm a diagnosis of fibromyalgia. Instead doctors work to rule out other possible causes of the symptoms such as vitamin and mineral deficiencies, multiple sclerosis, chronic fatigue syndrome, thyroid problems, Crohns disease, Lyme disease, and sleep apnoea; among others. This is achieved through physical exams and blood tests. MRIs or x-rays may also be used.
There is no single treatment option due to the complex nature of fibromyalgia and variations in how the condition presents itself. Most people with fibromyalgia use a combination of medications, diet, supplements, and physical therapies to manage the condition.
Psoriatic arthritis prevalence and symptoms
Psoriatic arthritis is a unique form of inflammatory arthritis closely associated with the condition psoriasis. The prevalence of this condition is not clearly known. Estimates suggest that between 0.3% and 1% have the condition6.
According to Arthritis Research UK, 2% of the population in the United Kingdom suffer from the skin disorder psoriasis, and approximately 14% of these people also have psoriatic arthritis7.
However, it’s also thought that this may be a conservative figure as psoriasis can sometimes go unrecognised or arthritis symptoms develop prior to psoriasis.
Both men and women are similarly at risk, with the disease commonly developing between the ages of 30 and 50.
Psoriatic arthritis symptoms
Psoriatic arthritis causes inflammation in the joints, causing them to become stiff, swollen and painful. It can affect any joint in the body, with symptoms varying from person to person. Psoriatic arthritis symptoms may developed rapidly and be severe, or the condition may develop slowing and only present mild symptoms.
Common symptoms include:
- Stiffness, swelling and pain associated with one or more joints.
- Stiffness and pain in the lower back, neck, or buttocks
- Pain in the tendons, usually affecting the sole of the foot or around the back of the heel
- Redness and discomfort around the eyes
- Changes in the colour and thickness of the toenails and fingernails
Two-thirds of people diagnosed with psoriatic arthritis will experience progressive joint degradation. Early diagnosis can help to slow the progress of the condition. Treatments usually involve anti-inflammatory medications and dietary changes. Some supplements many also help to alleviate inflammation and associated pain.
Systemic lupus erythematosus (SLE) prevalence and symptoms
Another autoimmune disease, systemic lupus erythematosus (SLE) affects the joints and connective tissues. It can also affect the brain, kidneys, skin and other organs.
This disease is more prevalent in women and people with Asian or African ancestry tend to be in a higher risk category. It’s estimated that there are 12.5-78.5 cases of SLE per 100,000 people in the United States and Europe, with a female to male ratio of 9:19,10.
Since this disease is rare, it’s difficult to determine incidence with great accuracy. However, it’s been estimated that there are around 2 and 7 new cases per 100,000 people diagnosed annually. Since it is a multisystem disorder, it can be very difficult to accurately diagnose.
Mortality associated with SLE has significantly decreased over the past 50 to 60 years due to better treatment options and earlier detection. Some people only experience mild symptoms, while others are at risk of life-threatening multi-organ failure.
SLE symptoms
There are many different symptoms associated with SLE. These can include swelling of the joints and associated pain, skin rashes, fever, appetite loss, sensitivity to sunlight, hair loss, lethargy, and weight loss.
Most people don’t experience all symptoms and how the disease will progress varies.
How SLE is treated will depend on the severity and disease manifestation. Anti-inflammatory medications, steroid creams, and corticosteroids are often used. Dietary changes and lifestyle adjustments are often necessary.
Ankylosing spondylitis prevalence and symptoms
It’s estimated that in the whole of Europe 1.3 to 1.56 million people suffer from ankylosing spondylitis (AS)8. The peak onset of AS usually starts between 20 and 30 years of age.
Unlike most other types of arthritis, AS affects more men than women. A chronic seronegative spondyloarthropathy form of arthritis, AS affects the axial skeleton.
Ankylosing spondylitis (AS) symptoms
Symptoms of AS are often subtle in the early stages, with the onset extending over several months to years. Many patients experience intermitted flares and periods of remission. Weight loss, fever, and fatigue are common symptoms during disease activity.
Inflammatory back pain is a key characteristic of this disease. The associated stiffness can interrupt sleep patterns and increase fatigue. The sacroiliac joints are the starting point for AS.
In advanced stages of the disease patients experience loss of lumbar lordosis and develop the ‘question mark posture’ as new bone growth around the spine joints causes permanent stiffness.
Although the spine is the main target of AS, this disease can also cause stiffness, inflammation and pain in other areas of the body such as the hips, ribs, shoulders, heels, and the small joints of the feet and hands. In some cases the eyes, heart, and lungs can be affected.
In a third of patients peripheral enthesitis develops, usually the behind the heel or the heel pad. These lesions are often painful and may be accompanied by swelling of the ligament or tendon.
Medication, diet, exercise, and supplements all play an important role in managing AS. Posture is particularly important to help avoid stiffness and flexion deformities of the spine. In severe cases surgery may be an option.
Gout prevalence and symptoms
This form of arthritis develops when monosodium urate crystals develop in the joints and other tissues. A common type of inflammatory arthritis, gout is more common in men than women. Studies show that the incidence of this disease is on the increase in the United Kingdom9.
Gout is very rare in people aged under 45, although it increases in prevalence with age.
According to statistics from Arthritis Research UK, gout affects 1.4% of adults in the United Kingdom.
Gout symptoms
Gout develops over four phases. Initially asymptomatic tissue deposition occurs. During this phase the deposition of urate crystals is occurring in the tissues, although there are no overt symptoms.
The second stage is characterised by acute flares in inflammation, resulting in swelling, redness, warmth, and pain of the affected joints. This may last for days or weeks and the pain can range from mild to excruciating. Gout is typically presented in the metatarsophalageal joint of the big toe.
A third stage in the disease progression is intercritical segments, where there are breaks between flares. As gout develops further into the final stage, patients tend to experience chronic arthritis. This leads to persistent soreness and aching of the joints.
Diet and lifestyle modifications are very important in the management of gout. There are also a range of medications and supplements which assist in the treatment of the condition.
Effectively managing arthritis
There are many different arthritis treatment options. Exercise is very important to help maintain joint flexibility and mobility.
Arthritis diets are also valuable to help reduce inflammation and minimise oxidative stress on the body. There are a variety of medications available specific to different types of arthritis, as well as key joint supplements that can help alleviate arthritis symptoms.
Supplements are a particularly effective way to support joint health and there is plenty of scientific research to confirm their effectiveness. However, products differ significantly in quality and value for money. Read our comparison of the top supplements for joint care to make informed choices.
Managing arthritis symptoms takes a multi-disciplinary response. While each patient will need a different approach based on the type of arthritis they have and their individual circumstances there are overarching themes.
Bibliography
- Murphy, L. et.al. (2008), Lifetime risk of symptomatic knee osteoarthritis. Arthritis and Rheumatism, Volume 59, Issue 9, (pp. 1207-12)
- Murphy, L. et.al. (2010). One in four people may develop symptomatic hip osteoarthritis in his or her lifetime. Osteoarthritis Cartilage, Volume 18, Issue 11, (pp.1372-9)
- Nyhall-Wahlin, B. et.al. (2006). Smoking is a strong risk factor for rheumatoid nodules in early rheumatoid arthritis. Annals of the Rheumatic Diseases. Volume 65, Issue 6, (pp. 601-6)
- DiFrancesco, L. (1994). Detailed immunohistologic evaluation of a methotrexate-induced nodule.Archives of Pathology & Laboratory Medicine. Volume 118, Issue 12, (pp. 1223-5)
- Thorne, J. et.al. (2007). Juvenile idiopathic arthritis-associated uveitis: Incidence of ocular complications and visual acuity loss. American Journal of Ophthalmology. Volume 143, Issue 5, (pp. 840-6)
- Gladman, D. et.al. (2005). Psoriatic arthritis: epidemiology, clinical features, course, and outcome. Annals of the Rheumatic Diseases. Volume 64, Issue 2
- Helliwell, P. (2009). Psoriatic arthritis: its presentation and management in primary care. In: “Hands On”, Series 6
- Dean, L. et.al. (2014). Global prevalence of ankylosing spondylitis. Rheumatology, Volume 53, Issue 4, (pp. 650-7)
- Kuo, C. et.al. (2013). Rising burden of gout in the UK but continuing suboptimal management: a nationwide population study. Annuals of Rheumatic Diseases, doi:10.1136/annrheumdis-2013-204463