SUMMARY
A large number of foods has been identified as rich in anti-inflammatory agents. These foods should be preferably consumed when an individual is suffering from arthritis.
There has been significant research into combination therapies that are making living with arthritis more manageable. In addition to medications, occupational therapy, and natural supplements, more people are subscribing to an arthritis diet consciously eating more of some foods and less of others.
What is inflammation and what causes it?
One of the underlying causes of the arthritic diseases is inflammation. When joints become inflamed they attract more inflammatory agents and white blood cells that cause further irritation. This causes the synovium (joint lining) to swell and leak into the surrounding tissues.
Medical Videos
And this is a technical video explaining in great detail specifically the pathology of joint inflammation:

Preventing and treating inflammation through diet
The relationship between diet and arthritis inflammation is a very important consideration in any patient’s diet plan. Food contains different nutrients and other compounds that can impact inflammation both positively and negatively.
Some substances will aggravate inflammation, while others can help to minimise inflammation. Understanding which foods to avoid and which foods to include in your diet for arthritis can make a significant difference.
One of the key considerations in any arthritis diet plan is to avoid foods that promote inflammation. This especially applies to people already diagnosed with rheumatoid arthritis, psoriatic arthritis, gout, lupus, or ankylosing spondylitis.
There are several key dietary recommendations for people with arthritis:
While these are good general guidelines, any arthritis diet should also focus on reducing inflammation, strengthening bones and cartilage, and reducing oxidative stress by elevating antioxidant intake.
Top foods and nutrients that reduce inflammation
Foods with omega-3 fatty acids
One key nutrient that is proving to be effective in reducing inflammation in sufferers of arthritis is omega-3 fatty acids.
Foods high in fibre
Foods rich in fibre help to fight inflammation by reducing the concentration of c-reactive protein. This protein is a marker of acute inflammation.
High levels of c-reactive protein are associated with patients suffering from arthritis.
In addition, studies also show that this protein is an important predictive marker for diabetes and cardiovascular disease5.
For these reasons alone, it’s highly recommended to have a high fibre diet6.
This will help to elevate arthritis symptoms, and it will also help to protect the body against other health problems.
Top 10 Fibre-Rich Foods
Foods high in vitamin B6
There has been a lot of research into the relationship between arthritis and B6. Also known and pyridoxine, this is one of eight B vitamins.
The body is unable to store B vitamins because they are water soluble.
Some studies have shown that people with rheumatoid arthritis have a higher requirement for B6 because inflammation reduces availablity7.
Supplementation with vitamin B6 has been found to significantly reduce the levels of pro-inflammatory compounds tumor necrosis factor –alpha (TNF-alpha) and interleukin-6 (IL-6)8.
Top 11 Fibre-Rich Foods
What is inflammatory arthritis?
Arthritis is a disease causing painful inflammation and stiffness of the joints. There are many different types of arthritis, the following five types of which are the most frequent ones:
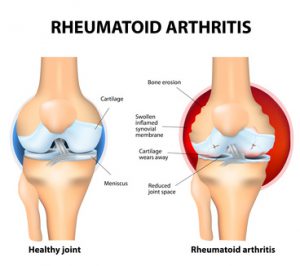
Rheumatoid Arthritis (RA) is an inflammatory type of arthritis that usually affects knees. Rheumatoid arthritis of the knee the auto immune disease. The body’s immune system mistakenly attacks healthy tissue.
After osteoarthritis, rheumatoid arthritis is the most common form of arthritis in the UK, affecting approximately 400, 000 people. Symptoms of this disease usually start to present themselves when the patient is aged between 40 and 50, although adults of any age can be affected.
Rheumatoid arthritis affects more women than men9.
Although the exact cause of rheumatoid arthritis is not fully understood, it’s known that the immune system has an abnormal response that promotes joint inflammation, attacking cartilage and other tissues around the joint. This progressively damages the joint and causes stiffness and discomfort, ultimately impeding function and movement
Gout is a form of inflammatory arthritis, which develops in response to an abnormal build-up of uric acid. The body is unable to effectively expel this substance, leading to crystallisation and deposition within the joints.
Gout is typically associated with the big toe; however the ankles, insteps, fingers, knees, wrists, heels, and elbows may also be affected.
People that have the skin condition psoriasis are at risk of developing psoriatic arthritis. Although there are variations in symptoms, inflammation is very common and can cause significant pain and discomfort.
There are several classifications of lupus, although they all related to tissue swelling associated with an abnormal auto-immune response. Systemic lupus erythematosus is especially detrimental to joint health.
Predominately associated with the spine, ankylosing spondylitis is a chronic inflammatory arthritis characterised by back stiffness and pain. Over time it can lead to ankylosis. Often other parts of the body are also affected by inflammation including the hip, shoulders, ribs, and hand and feet joints.
How common is arthritis and what are the symptoms?
There are approximately 10 million people in the UK alone suffering from some form of arthritis. This disease of the musculoskeletal system presents itself in a wide range of form, with over 100 different classifications.
In general, arthritis symptoms include joint inflammation, stiffness, pain, and impaired function.
There are a wide range of joints and surrounding tissues that can be affected, eventually leading to joint instability, deformation, and lack of mobility if not properly managed.
Unfortunately, at this stage there is no 100% cure for any type of arthritis, including the prevalent osteoarthritis and rheumatoid arthritis.
Sourcing anti-inflammatory nutrients
There are essentially two ways to source the above nutrients: from high quality, whole foods or from food supplements.
On the one hand, sourcing the nutrients from whole food will guarantee that you will eat a more balanced and complete diet on the whole. On the other hand, however, it is both cost and time-intensive to ensure that all nutrients are supplied every day in sufficient dosages.
Fresh, unprocessed high quality foods need to be purchased from markets to minimise occurrence of preservatives and toxins. Of course, these pollutants in cheap food can themselves aggravate inflammation.
Food supplements are more efficient and effective at supplying the nutrients. Of course, patients should do their utmost to follow a healthy arthritis-friendly diet in any case.
Video & list: the inflammatory foods you MUST avoid
Everybody will react differently to various foods and there is no “perfect” arthritis diet. However, many people with arthritis should foods that are known to irritate inflammation.
[box title=”Arthritis Diet Foods To Avoid” box_color=”#f0182c”]• Sugar • Refined Carbohydrates • Alcohol • Saturated & Trans Fats • Gluten • Nightshades [/box]
Watch this short video for the 5 worse foods for arthritis

Conclusion
A large number of arthritis-friendly foods have been identified and these should be preferably consumed. At the same time it is advisable to consume so-called combination joint supplements to ensure that the micro nutrients are available to the body in effective dosages.
Bibliography
- “Artemis, P. and Simopoulos, M. (2002). Omega-3 fatty acids in inflammation and autoimmune diseases. Volume 21, Issue 6.
- “Geusens, P. et.al. (2005). Long-term effect of omega-3 fatty acid supplementation in active rheumatoid arthritis. Volume 37, Issue 6, (pp. 824-9).
- “Yan, Y. et.al. (2013). Omega-3 fatty acids prevent inflammation and metabolic disorder through inhibition of NLRP3 inflammasome activation. Immunity, Volume 38, Issue 6, (pp. 1154-63).
- “Calder, P. (2013). Omega-3 polyunsaturated fatty acids and inflammatory processes: nutrition or pharmacology? British Journal of Clinical Phamacology. Volume 75, Issue 3, (pp. 645-62).
- “Yunsheng, M. et.al. (2006). Association between dietary fiber and serum C-reactive protein. The American Journal of Clinical Nutrition. Volume 83, Issue 4, (pp. 760-6).
- “Ajani, U. et.al. (2004). Dietary fiber and C-reactive protein: findings for national health and nutrition examination survey data. Volume 134, Issue 5, (pp. 1181-5).
- “Friso, S. et.al.(2001). Low circulating vitamin B(6) is associated with elevation of the inflammation marker C-reactive protein independently of plasma homocysteine levels. Circulation. Volume 103, Issue 23, (pp. 2788-91).
- “Huang, et.al. (2010). Vitamin B6 supplementation improves pro-inflammatory responses in patients with rheumatoid arthritis. European Journal of Clinical Nutrition, Volume 64, (pp. 1007-13).
- “Crowson, C. et.al. (2011). The lifetime risk of adult-onset rheumatoid arthritis and other inflammatory autoimmune rheumatic diseases. Arthritis and Rheumatology, Volume 63, Issue 3, (pp. 633-9).